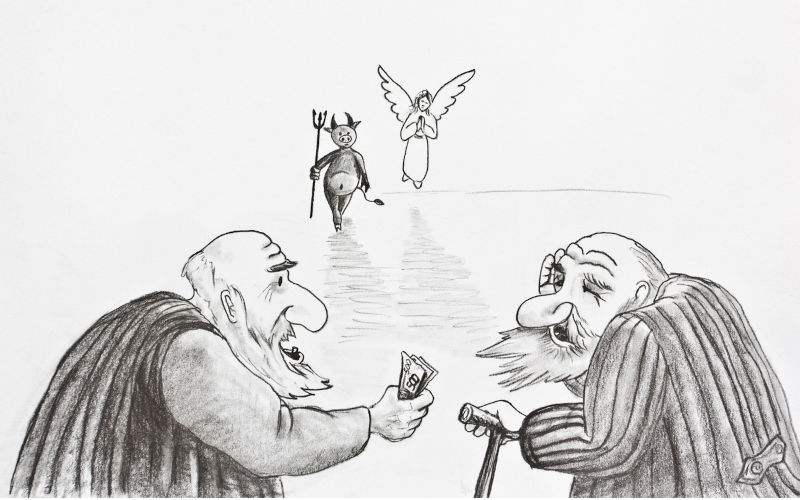
Allied health devil in aged care reform detail
May 6, 2025
As Kathy Eagar discussed, positive reforms to the Australian aged care system are somewhat undercut by bigger costs for older people and increasing privatisation via the new Support at Home program.
At first glance, two welcome developments are the government commitment to 100% funding clinical care in residential and home aged care, and acknowledgement of the importance of “reablement” and multidisciplinary team care under Support at Home.
These changes are consistent with the Aged Care Royal Commission’s identification of reablement — maintaining or regaining function and reducing or preventing functional decline — as critical to older people’s health and well-being. The commissioners criticised the pitiful amount of allied health service provision (now even lower) and recommended that aged care include a level of allied healthcare appropriate to each person’s needs.
But in residential care, there will continue to be no dedicated funding for allied health services, with providers expected to pay for them out of their overall direct care funding. And there are no benchmarks for allied service provision, unlike mandatory minimum minutes for personal and nursing care. Allied health needs assessment processes are also inconsistent, so we cannot even estimate how much ought to be provided.
Providers prioritise their care minute targets. Not being held to account for allied healthcare, they may not even spend what is left on direct care, instead using it to subsidise other costs like everyday living and accommodation. Despite the Royal Commission’s recommendation that allied healthcare should generally be provided by aged care providers, this situation is likely to persist as long as there is no clarification of who should be responsible.
To make matters worse, proposed changes to the Aged Care Rules retain an option for providers to simply provide “access” to allied healthcare. They then do not have to pay for it in any way, even for transporting the resident to an appointment. Although there is also an option to develop and pay for an allied health program for a resident, it isn’t at all clear how providers decide which option to choose, and they are not held to account by the aged care regulatory system.
Allied health professionals are aware of many instances where the only allied health service offered to residents is physiotherapy, which even then may only be available in group sessions. When residents or their family members request other allied health services, they are told the facility does not provide them and that they will have to find them.
Older people and their families must then seek these allied health services through Medicare, Veterans’ Care, private insurance, or state and territory health services. These pathways external to the aged care system do not come close to meeting residents’ allied healthcare needs, because of limited access to the various avenues, restrictions on the amount and type of care that can be obtained, and — increasingly — gap fees and limited rebates. With the only other choice being to pay the whole cost themselves, many people simply do not pursue recommended treatment. Promising to pay 100% of clinical care costs starts to look like bad faith in this context.
Support at Home is better in this respect. But again it pays to read the fine print. To be funded by government, services must be listed in the Aged Care Rules, which in their last public iteration included less than half of the different allied health professions in aged care, excluding services such as orthotics and prosthetics. Osteopathy, chiropractic and art therapy are also not defined as clinical care, but instead listed under “Therapeutic services for independent living” which can require a means-tested “consumer” contribution of up to 50% of the cost.
It is good news that Support at Home includes a new Assistive Technology and Home Modifications scheme. However, a new lifetime cap of $15,000 for home modifications is unrealistic, as it will exacerbate economic inequity and ultimately work against the government’s policy of encouraging older people to stay safely living at home for as long as possible.
And as for services more generally under Support at Home, careful reading of the accompanying manual shows that any “consumer” co-contribution is considered as part of the overall budget for that tier of service. For example, prescription of assistive technology or home modifications by an occupational therapist or speech therapist, and associated “wrap around” support, are provided at no cost to the consumer (being defined as clinical care), but the cost of this is considered to be a part of the total AT-HM budget.
The technology or building modification provided is considered as part of the “Independence” category and, therefore, the older person may have to pay up to 50%. Any such co-contribution is also regarded as part of the person’s overall AT-HM budget, as are the provider’s assistive technology administration and home modification co-ordination costs.
The 16-week Restorative Care Pathway is the part of Support at Home that is the most strongly linked to reablement and identifies allied healthcare as central to it. Consistent with Royal Commission recommendations, multidisciplinary care is represented in the Support at Home manual as a critical element of the Pathway. However, there is a big question mark over how associated necessary processes such as shared protocols and conferences are to be funded. And the new regulatory system does not include any obligation on Support at Home providers to actually provide multidisciplinary care.
There will also be limited places allocated for the Restorative Care Pathway. So it is likely that the current significant wait times for Home Care Packages will also be reality for some older people who have been assessed to need restorative care under Support at Home, even if they are allocated a Support at Home classification tier.
Outside the Restorative Care Pathway, the manual makes very little reference to allied healthcare, and yet again we are left waiting for more information.