This month, support Pearls and Irritations with your tax deductible donation
We continue to see powerful interests shape the headlines and spread misinformation faster than facts in current times. This year, Pearls and Irritations has again proven that independent media has never been more essential. We have continued to push the issues ignored by mainstream media, building our voice as a trusted source for local and global issues. We ask you to support our plans for 2026.
For the next month you can make a tax deductible donation through the Australian Cultural Fund via the link below.
Donate
5 December 2025
Fear versus facts: why migrants strengthen Australia
Australia’s multicultural society is not a modern experiment or a social crisis. It is the product of shared effort, grounded in First Nations custodianship and strengthened by generations of migrants who have helped build the nation’s economy, culture and community life.

5 December 2025
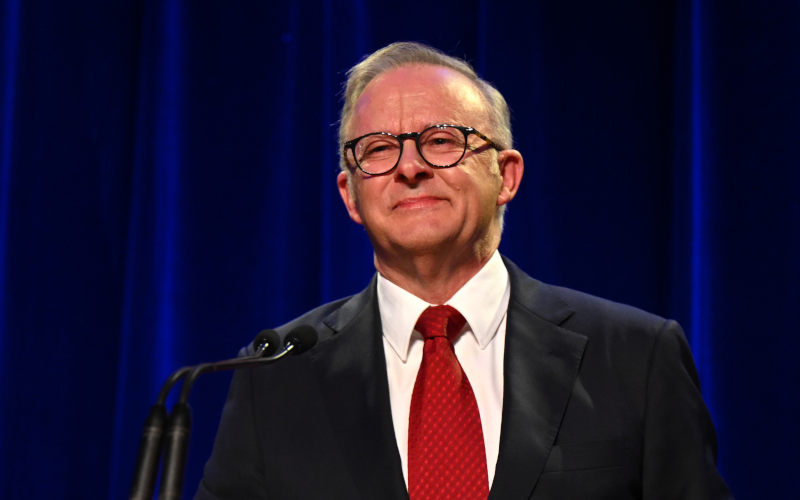
Words or action? Dreyfus and human rights at home
Mark Dreyfus has been appointed Australia’s special envoy on human rights. Is the government prepared to match international advocacy with concrete action at home – by finally legislating a Human Rights Act?

5 December 2025
When foreign policy becomes domestic theatre
Australia’s response to Japan’s rhetoric has been framed as a test of loyalty, but the outrage is largely media-driven. Caution in foreign policy is not betrayal – it is a rational defence of national interest.
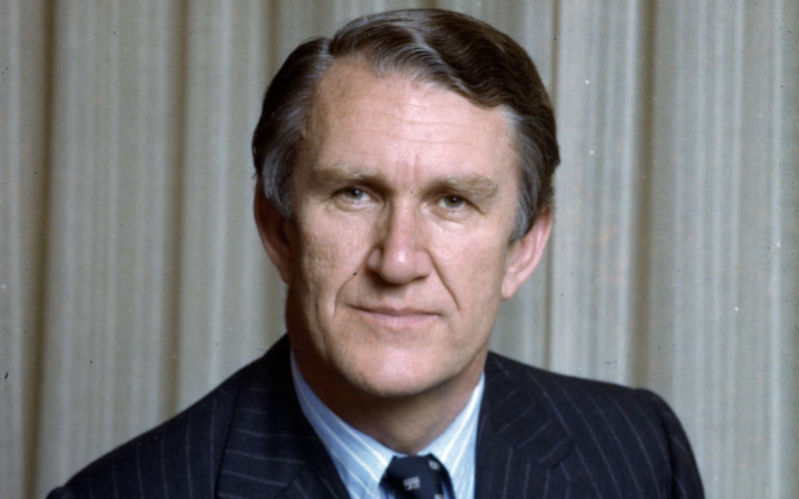
Launching Pearlcasts
The 50th Anniversary of the Dismissal of the Whitlam Government
We kick off with a topic close to our hearts, the 50th anniversary of the Dismissal of the Whitlam Government. We have three of the best sources in the nation taking part: our editor-in-chief John Menadue – the living link to the scandal and the nation’s top public servant at the time; Jenny Hocking, author of The Palace Letters and Australia’s pre-eminent Dismissal historian; and Brian Toohey, the journalist who has dug deepest into the darkest elements of the events.
Go to Pearlcasts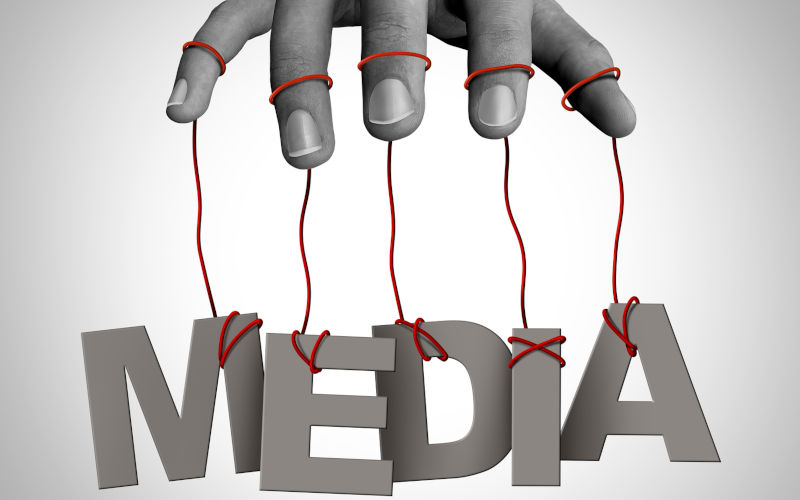
5 December 2025
How media coverage helps normalise the far right
Media coverage does more than report on the far right. Through language choices, sensationalism and false balance, journalism can help shift racist politics into the mainstream.

5 December 2025
Trump’s drug war on Venezuela reeks of hypocrisy
Donald Trump’s campaign against Venezuela is less about drugs than power, exposing deep hypocrisy in US policy and raising uncomfortable questions for Australia about its alliance.

5 December 2025
Is the focus on NAPLAN’s ‘top’ schools a good idea?
This year’s NAPLAN results reveal encouraging stories of student progress, but headlines about 'top' schools risk oversimplifying how improvement really happens – and what parents should take from the data.

5 December 2025
A Boyer Lecture that misunderstands Australia’s defence history
The latest Boyer Lecture portrays Australia as trapped by anxiety about the United States. In fact, for decades the country pursued a deliberate, bipartisan strategy of defence self-reliance – abandoned only in recent years.
5 December 2025
Celebrating war crimes is a moral failure, not cultural pride
From ancient Rome to modern Melbourne, societies have repeatedly transformed civilian suffering into spectacle. Celebrating violence against the innocent is not a cultural quirk – it is a profound moral collapse.

5 December 2025
Corruption prosecutions are choking Indonesia’s reform ambition
High-profile prosecutions of Indonesia’s technocrats are reshaping incentives across government and business. When good-faith decisions are treated as crimes, reform, investment and innovation all suffer.
5 December 2025
Book Review: Selling Israel: propaganda, history and contested narratives
Harriet Malinowitz’s Selling Israel examines how Zionist ideology has been promoted through propaganda, history and selective memory, and why separating Judaism from Zionism matters in confronting antisemitism.

4 December 2025
Australia’s immigration 'debate' is rhetoric, not policy
Australia is awash with immigration rhetoric, but little of it is grounded in evidence, clear definitions or serious policy alternatives. Rather than an informed public debate, Australians are being offered slogans, blame and ambiguity.
Latest on Palestine and Israel
5 December 2025
Book Review: Selling Israel: propaganda, history and contested narratives
Harriet Malinowitz’s Selling Israel examines how Zionist ideology has been promoted through propaganda, history and selective memory, and why separating Judaism from Zionism matters in confronting antisemitism.

3 December 2025
Global campaign amplifies call for the release of jailed Palestinian leader Barghouti
An international campaign is calling for the release of Palestinian political figure Marwan Barghouti, arguing his freedom could reshape Palestinian politics and revive peace efforts.

3 December 2025
What charges does Benjamin Netanyahu face, and what’s at stake if he is granted a pardon?
Benjamin Netanyahu has requested a pardon while still on trial for corruption. The move raises serious questions about legal accountability, judicial independence and political survival.

1 December 2025
‘Genocide is not over,’ Amnesty leader says as Israel keeps bombing Gaza
“So far, there is no indication that Israel is taking serious measures to reverse the deadly impact of its crimes and no evidence that its intent has changed.”

29 November 2025
Gaza’s true death toll could be 126,000 or even higher
New research suggests Gaza’s death toll may be far higher than widely reported, with devastating implications for life expectancy, poverty and accountability.

25 November 2025
The ceasefire that isn’t: 400 violations in 40 days
Israel has violated the ceasefire in Gaza hundreds of times since October, using vague or unverified justifications to carry out strike in a recurring pattern of escalation and impunity.

23 November 2025
The UN embraces colonialism: the Security Council and the US Gaza plan
The Security Council's backing of the Trump plan for Gaza ignores international law, punishes the Palestinians, and rewards those responsible for genocide.

21 November 2025
UN Members complicit in genocide
UN Special Rapporteur on Palestine Francesca Albanese discusses why, in her most recent report, she called out more than 60 nations for their collective-crime roles in the ongoing genocide in Gaza.

Israel's war against Gaza
Media coverage of the war in Gaza since October 2023 has spread a series of lies propagated by Israel and the United States. This publication presents information, analysis, clarification, views and perspectives largely unavailable in mainstream media in Australia and elsewhere.
Download the PDFLatest on China

5 December 2025
When foreign policy becomes domestic theatre
Australia’s response to Japan’s rhetoric has been framed as a test of loyalty, but the outrage is largely media-driven. Caution in foreign policy is not betrayal – it is a rational defence of national interest.

1 December 2025
How soybeans became a fault line in China’s food security
China now buys 60 per cent of the world’s soybeans. That dependency shapes its food security strategy – and its trade battles with the United States.

30 November 2025
New architecture, old assumptions: Australia and the China question
Foreign Minister Penny Wong speaks of balance, equality and a new regional order – yet Australia’s China policy still carries Cold War assumptions that risk strategy, prosperity and peace.

Support our independent media with your donation
Pearls and Irritations leads the way in raising and analysing vital issues often neglected in mainstream media. Your contribution supports our independence and quality commentary on matters importance to Australia and our region.
DonateMore from Pearls and Irritations
Latest letters to the editor
Sir Humphrey and international law
Les Macdonald — Balmain NSW 2041
A simple solution
Les Macdonald — Balmain NSW 2041
Can he stay or will he go
Hal Duell — Alice Springs
Government funding of private schools should be phased out
Elizabeth Sprigg — Glen Iris, Victoria