
10 July 2025
The story most Israelis are not allowed to hear
I write this in quite a distressed state. On Sunday, I watched the award-winning documentary film – “No Other Land”.

10 July 2025
Australia obstructed probe into deadly ‘Rainbow Warrior’ bombing
France's ‘Operation Satanique’ bombing of the Greenpeace ship Rainbow Warrior, 40 years ago this month, was state-sponsored terrorism – and Australia had a part in helping French secret agents to escape.

10 July 2025
Israeli defence minister orders plan to build concentration camp for Gaza’s civilian population
Israel Katz says the so-called humanitarian city will be built on the ruins of Rafah.

Support our independent media
Pearls and Irritations is funded by our readers through flexible payment options. Choose to make a monthly or one off payment to support our informed commentary
Donate
10 July 2025
Who wants to serve on a jury? Is the jury system still the best we can do?
You may have been following the current criminal trial in Victoria where a woman is accused of murdering three people by serving them a meal laced with death cap mushrooms.

10 July 2025
'Indefensible': Trump budget law subsidises private jet owners while taking healthcare from millions
A provision of the budget law that President Donald Trump signed last week will leave taxpayers to pick up the tab for the private jet industry and billionaire high flyers.

10 July 2025
Tariff deadline extended as Trump’s trade talks falter
It was supposed to be 90 trade deals in 90 days, turbocharged by the threat of ‘Liberation Day’ tariffs.

10 July 2025
The housing crisis is everyone's problem
The housing crisis has been decades in the making but we cannot afford decades to solve it.

10 July 2025
Anti-tourism protests are not new. They happened in ancient Rome, 19th-century England and after World War II
This hot European summer, anti-tourism protests have made headlines, from Barcelona to Venice, Mallorca and the Canary Islands. The unrest is not confined to Europe, though.

10 July 2025
Empathy, morality, civilisation and resisting tyrants
Are we just selfish brutes who need to be civilised into social, moral behaviour? If not, where do our decency and altruism come from? Can we resist the tides of fear and control rolling over us and cultivate more compassionate and peaceable societies?

10 July 2025
The end of multilateralism
The recent unilateral strikes by the United States on Iran’s nuclear development sites underline the fact that multilateralism is dead, and has been so for some time.
9 July 2025
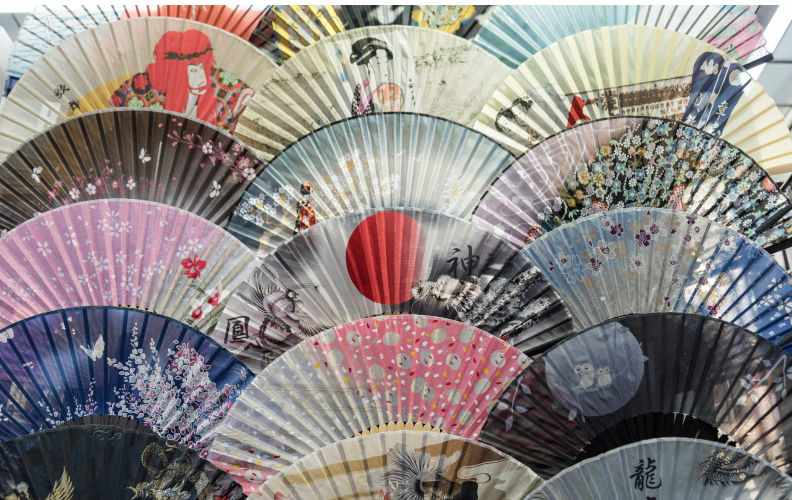
Missed opportunities in Japan
John Menadue points to the lack of Australian interest and involvement in Asia.
Latest on Palestine and Israel

10 July 2025
The story most Israelis are not allowed to hear
I write this in quite a distressed state. On Sunday, I watched the award-winning documentary film – “No Other Land”.

10 July 2025
Israeli defence minister orders plan to build concentration camp for Gaza’s civilian population
Israel Katz says the so-called humanitarian city will be built on the ruins of Rafah.

9 July 2025
Freedom of speech and chants
“Death, death to the IDF [Israel Defence Forces]” and “Death, death to the IOF [Israeli Occupying Force]”. Chants that some in the Palestinian support movement in Melbourne used last weekend.

9 July 2025
Punishment, proportionality and principle
The reaction to the fire bombing on a Jewish establishment in Melbourne has been sadly predictable.

8 July 2025
The one-word problem for Israel
The massive, almost universal, support nations have provided Israel since the Hamas attacks is eroding around the world and new research indicates that most people surveyed over 24 countries now have negative views of Israel and Netanyahu.

8 July 2025
When the helping hand holds a machine gun
There’s no precise number of how many Palestinians have been starved to death by Israel’s embargo on food entering Gaza.

7 July 2025
J’accuse (Part 2) – The Israel lobby
Readers may recall a piece published here on Pearls and Irritations (J’accuse!... the Jew who accuses his fellow Jews of being antisemites on 23 February, 2025 — in which I wrote about an offensive tweet Mark Leibler (lawyer and leader of AIJAC) posted on X — in which, amongst other things, he described those Jews criticising Israel as “vicious antisemites”.

6 July 2025
Gunning for the Greens over Gaza - Part 1
After the federal election on 3 May, dissection of the Liberals’ turmoil received top billing.

Israel's war against Gaza
Media coverage of the war in Gaza since October 2023 has spread a series of lies propagated by Israel and the United States. This publication presents information, analysis, clarification, views and perspectives largely unavailable in mainstream media in Australia and elsewhere.
Download the PDFLatest on China

9 July 2025
Trump’s budget and the 21st century great divergence
Donald Trump’s recently passed budget has the capacity to lay the foundation for a widening gap between the world's two largest economies, the United States and China, and make China as great, comparatively, as it was before the industrial revolution.

8 July 2025
China and renewable energy: The global impact
China’s renewable energy program is not a local curiosity. It marks a turning point in history with profound consequences for the rest of the globe.

4 July 2025
China’s rapid adoption of AI demands greater scrutiny of the social impact
In contrast to the perception that Beijing has placed a lot of guardrails on AI, China’s AI regulation so far has been limited.

Support our independent media with your donation
Pearls and Irritations leads the way in raising and analysing vital issues often neglected in mainstream media. Your contribution supports our independence and quality commentary on matters importance to Australia and our region.
DonateMore from Pearls and Irritations
Latest letters to the editor
Repetition does not validate a falsehood
Richard Llewellyn — Colo Vale
Being an 'expert' doesn't mean I don't get my view
Steve M — Brisbane
We need fewer people and renewable food
Julian Cribb — Canberra, ACT
Incitement to criminal law
Rick Pass — Rifle Creek FNQ






