This month, support Pearls and Irritations with your tax deductible donation
We continue to see powerful interests shape the headlines and spread misinformation faster than facts in current times. This year, Pearls and Irritations has again proven that independent media has never been more essential. We have continued to push the issues ignored by mainstream media, building our voice as a trusted source for local and global issues. We ask you to support our plans for 2026.
For the next month you can make a tax deductible donation through the Australian Cultural Fund via the link below.
Donate
15 December 2025
A beginners guide to Australian aged care policy in 2025
Stereotypes about wealthy baby boomers are skewing aged care policy. New fees, the shift to Support at Home, and pressures on community services risk leaving many older Australians without affordable, safe support. The consequences will be felt across families, hospitals and future generations.

15 December 2025
Message from the Editor
As we hurtle towards the chaos of Christmas, we are taking a moment to reflect on the high and lows of 2025, and what it all means for 2026.

15 December 2025
Conflicts, corrections and confusion: pressure mounts on the NACC Commissioner
The Inspector of the NACC has received 90 complaints since 1 July. Most of these complaints concern the NACC Commissioner’s conflict of interests with Defence.
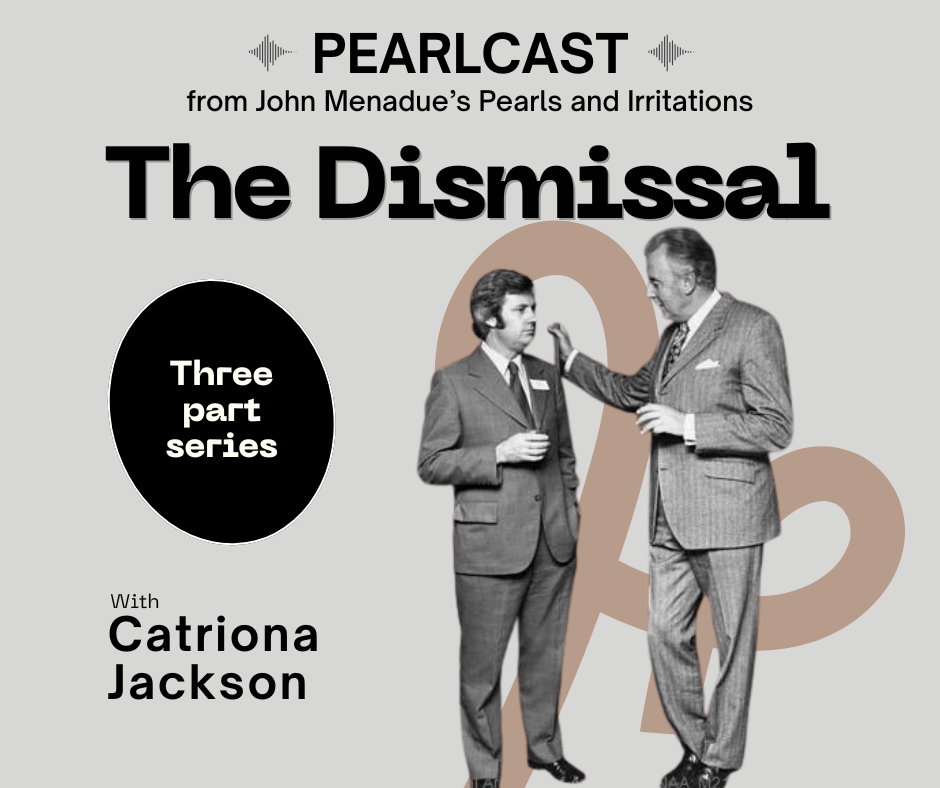
Launching Pearlcasts
The 50th Anniversary of the Dismissal of the Whitlam Government
We kick off with a topic close to our hearts, the 50th anniversary of the Dismissal of the Whitlam Government. We have three of the best sources in the nation taking part: our editor-in-chief John Menadue – the living link to the scandal and the nation’s top public servant at the time; Jenny Hocking, author of The Palace Letters and Australia’s pre-eminent Dismissal historian; and Brian Toohey, the journalist who has dug deepest into the darkest elements of the events.
Go to Pearlcasts
15 December 2025
Trump’s empire of hubris and thuggery
Donald Trump's latest National Security Strategy memorandum treats the freedom to coerce others as the essence of US sovereignty. It is an ominous document that will – if allowed to stand – come back to haunt the United States.

15 December 2025
If government won’t deliver reform, citizens can
Governments routinely ignore expert advice and community lobbying. Caroline Fitzwarryne argues that Australians must organise, draft reforms and lead practical projects themselves, rather than waiting for politicians to act.

15 December 2025
Book Review: Merlinda Bobis explores four generations of colonialism and violence in the Phillipines
Merlinda Bobis’ In the Name of the Trees weaves four generations of Bikol women into a powerful exploration of colonial violence, language, land and survival.

15 December 2025
The next century will be shaped by resistance, not inevitability
Across six centuries, power has claimed inevitability while resistance has redrawn the possible. As the world enters a century defined by climate, inequality and democratic strain, the forces that push back from below may once again shape the future.

14 December 2025
Would Donald Trump pass an Australian Values test?
As the Coalition considers adding an Australian Values test to the Character Test, Abul Rizvi asks a simple question: what happens when you apply it to someone whose behaviour is extensively documented – like Donald Trump?

14 December 2025
Book extract: Understanding China: governance, socio-economics, global influence
China’s rise has reshaped global economics, lifted millions out of poverty, and challenged Western assumptions about governance. This extract from 'Understanding China, Governance, Socio-Economics Global Influence' argues that engagement, not confrontation, offers the only viable path forward.

14 December 2025
Degrowing the economy for people and planet
Imperialism, colonialism, racism and ecocide: the four horsemen of capitalism’s apocalypse? Climate change threatens the survival of migratory species, and China continues to dominate the supply of rare earth elements.

14 December 2025
How charitable are Australians? Three charts show how much we give
New data shows fewer Australians are claiming tax-deductible donations and our global ranking for generosity is slipping. Changing giving habits, the rise of online fundraisers and an ageing donor base all help explain what the statistics miss.
Latest on Palestine and Israel
5 December 2025
Book Review: Selling Israel: propaganda, history and contested narratives
Harriet Malinowitz’s Selling Israel examines how Zionist ideology has been promoted through propaganda, history and selective memory, and why separating Judaism from Zionism matters in confronting antisemitism.

3 December 2025
Global campaign amplifies call for the release of jailed Palestinian leader Barghouti
An international campaign is calling for the release of Palestinian political figure Marwan Barghouti, arguing his freedom could reshape Palestinian politics and revive peace efforts.

3 December 2025
What charges does Benjamin Netanyahu face, and what’s at stake if he is granted a pardon?
Benjamin Netanyahu has requested a pardon while still on trial for corruption. The move raises serious questions about legal accountability, judicial independence and political survival.

1 December 2025
‘Genocide is not over,’ Amnesty leader says as Israel keeps bombing Gaza
“So far, there is no indication that Israel is taking serious measures to reverse the deadly impact of its crimes and no evidence that its intent has changed.”

29 November 2025
Gaza’s true death toll could be 126,000 or even higher
New research suggests Gaza’s death toll may be far higher than widely reported, with devastating implications for life expectancy, poverty and accountability.

25 November 2025
The ceasefire that isn’t: 400 violations in 40 days
Israel has violated the ceasefire in Gaza hundreds of times since October, using vague or unverified justifications to carry out strike in a recurring pattern of escalation and impunity.

23 November 2025
The UN embraces colonialism: the Security Council and the US Gaza plan
The Security Council's backing of the Trump plan for Gaza ignores international law, punishes the Palestinians, and rewards those responsible for genocide.

21 November 2025
UN Members complicit in genocide
UN Special Rapporteur on Palestine Francesca Albanese discusses why, in her most recent report, she called out more than 60 nations for their collective-crime roles in the ongoing genocide in Gaza.

Israel's war against Gaza
Media coverage of the war in Gaza since October 2023 has spread a series of lies propagated by Israel and the United States. This publication presents information, analysis, clarification, views and perspectives largely unavailable in mainstream media in Australia and elsewhere.
Download the PDFLatest on China

14 December 2025
Book extract: Understanding China: governance, socio-economics, global influence
China’s rise has reshaped global economics, lifted millions out of poverty, and challenged Western assumptions about governance. This extract from 'Understanding China, Governance, Socio-Economics Global Influence' argues that engagement, not confrontation, offers the only viable path forward.

7 December 2025
Ceding the future to China
Delivered as remarks to Brown University’s Watson School during its “China Chat” series, Chas Freeman reflects on China’s return to global prominence and the United States’ accelerating retreat from the international order it once led – and asks what coexistence looks like as power shifts in the 21st century.

6 December 2025
China’s challenge is explaining why it succeeded
Western commentary often dwells on China’s problems while overlooking the cultural and historical foundations of its extraordinary achievements. Understanding both is essential to informed judgement.

Support our independent media with your donation
Pearls and Irritations leads the way in raising and analysing vital issues often neglected in mainstream media. Your contribution supports our independence and quality commentary on matters importance to Australia and our region.
DonateMore from Pearls and Irritations
Latest letters to the editor
Let the facts speak for themselves
Les Macdonald — Balmain NSW 2041
And have a guess who is responsible?
Les Macdonald — Balmain NSW 2041
Memo to Albanese: still a little left to destroy
Richard Llewellyn — Colo Vale
Climate and the pursuit of capital
Fiona Colin — Melbourne