PETER BROOKS, STEPHEN DUCKETT and BRIAN OLDENBURG. Telehealth and digital health navigators – a bright future.
Jun 8, 2020Telehealth is not new in Australia but Covid -19 and the new Medicare item numbers have stimulated its rapid adoption across the country. It is clear patients like it. They do not need to expose themselves to potentially dangerous environments such as hospitals and clinics. It saves them time whether in rural or urban environments and it delivers care – and patient education, in their own environment.
Appropriate models of ‘virtual ‘care delivery need to be refined and appropriately funded with Medicare item numbers that are robust and include a wide range of services and individual health professionals. Telehealth will make a big difference to care delivery around the world with a ‘new’ digitally enabled health workforce needing to be trained. In Australia we must not revert to the health system we had pre Covid-19.
Of the many changes to everyday life during the COVID-19 pandemic has been the massive growth in billed telephone consultations and video consultations. The majority seem to be voice or text but the public have lapped up this new way of interacting and getting advice. After the pandemic, the health system – professionals and payers – need to institutionalise tele-health as a valid, useful and efficient part of the new health system.
Australia, especially Queensland with its dispersed population over vast distances, has been a leader in telehealth implementation and research for many years. The Queensland Telehealth Unit has supported local telehealth initiatives, de-emphasising adoption of the latest technology, in favour of developing systems and processes which make telehealth sustainable within the budgets of local health services e.g. showing that telehealth implementation can reduce patient transport costs met by the hospital. The University of Queensland based Centre for Research Excellence in Telehealth supported cutting edge innovation and evaluation to show what worked and what didn’t. And this has helped inform a significant cultural change to adopt Telemedicine broadly across Queensland Health facilities. Other Australian states such as WA have already adopted a plan to convert 30-40% of outpatient attendances to virtual consultations over the next few years.
Interestingly other countries have been much more open to embracing telehealth in their health systems. In the US, over 50% of some 100 million consultations undertaken by Kaiser Permanente were by telehealth and the Veterans Affairs system – which provides care to 10 million Veterans – used telehealth in over 70 % of interactions and managed to make this change from around 10% use of telehealth over a 3-year period.
It is not that there has been no interest in telehealth in Australia over the past 20 years; rather, it is just that uptake has been incredibly slow and unsupported until the last 6 weeks with the introduction of a range of new telehealth item numbers primarily for Doctors and nurses and Allied health professionals Interestingly, although the traditional telephone was supposed to be the back-up if video were not available, telephone appears to be the dominant medium used with the new items.
In this last 2 months many hospitals and health professionals are now doing over 50% of their interactions with patients ‘virtually ‘- and it took Covid-19 to make us change our (health professionals) behavior.
If these recent sudden changes are to be maintained in the future, it is important that health consumers are also supported in this ‘brave new world’ and that more effort is put into using video and more contemporary technology to manage complex chronic conditions at home. This change, while driven by technology, has to be a cultural change- but it does require leadership and recognition that we need to engage consumers in decisions around the type of health care they want and how they want it delivered. Telehealth provides a real opportunity for genuine ‘patient participation ‘ in clinical decision making and in engaging patients in designing a health system that works for them as well as for health professionals and the payers.
Think, for example, the real savings ( financial and time – which also has a monetary value) to be gained by using Telehealth when it takes around 2- 2.5 hours and significant costs for transport and parking ( let alone a contribution to carbon emissions ) to keep a 20 minute health care appointment in the middle most cities in Australia,. We know the benefits of Telehealth to the rural /remote sector – we need to accept them in urban settings as well.
Telehealth can also be used for patient and professional education, for expanding the reach of clinical trials so that those in rural areas have same access to new therapies as those living in our major population centres, home monitoring and many other health related activities including patient education.
As we emerge from the current ‘social distancing’ phase, it will be important to look at all of the ways in which health care can be delivered more effectively and efficiently to health consumers by using available technology. The Covid-19 crisis has exposed important weaknesses with our current health care system which we should address and one of those is how we are going to utilize digital solutions including Telehealth for the benefit of all in the health system. Think what a difference this will make to Hospitals – they may become smaller, more focused of high technology interventions as in Denmark and other Scandinavian countries. The Topol Review provided for Health Education England delivers an excellent road map of what can be achieved by using this technological revolution not just for health professionals but for patients, carers and the wider community . Use of Chat Bots , AI (artificial Intelligence) driven solutions and as range of monitoring devices will all be in the ‘MIX “.
Importantly these changes will require a significant change in the health workforce
In providing them with technology skills.
Development of new roles – digital health technicians (who will be key part of any clinical practice in the future) to ensure health professionals and patients can connect rapidly with each other at any virtual consultation.
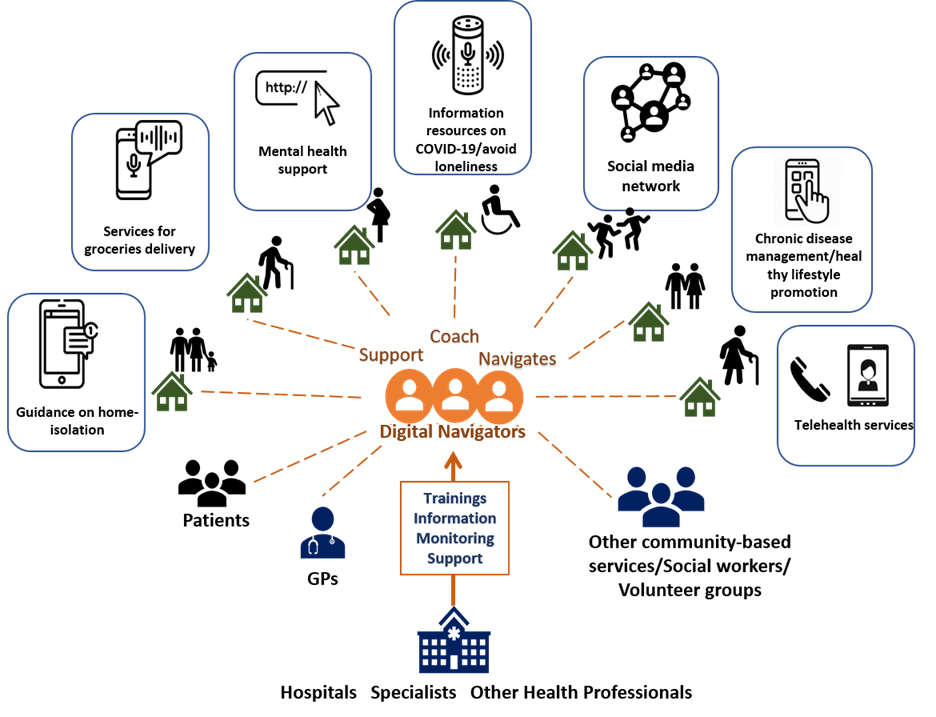
Digital health navigators who can guide patients to the information they require to assist them better manage their chronic diseases in a safe environment – their homes and communities
Technology is key, but so is a human interface and this is where navigators can enhance and improve the experience and productivity of the digital health ‘revolution’. It may well be that social distancing will continue into the future and many isolated individuals will have difficulty managing their chronic health conditions, getting their medications, obtaining food, exercising, and maintaining their social and family connections. Many people do not have the digital literacy, knowledge of or access to the tools and resources to help them navigate through these complexities in order to find the required services, resources and supports.
The Navigators, assisted by AI-powered triage tools, deliver personalized care plans to help individuals deal with their social, health and mental health challenges. Tailored care plans comprising community-based solutions are determined based on an individual’s location, age, education level and health insurance status.
While designed to improve people’s quality of life Digital Navigators is also likely to save jurisdictions from rising healthcare costs of untreated medical and behavioural health problems. And this current crisis could provide job training coupled with employment opportunities in the burgeoning health sector, playing a role in alleviating the burden of rising unemployment due to this crisis and its significant impact on service industries.
To reap the full benefits of this opportunity to re imagine health care we need a framework that can ensure appropriate range and connectivity of technologies at both ‘ends’ of the consultation and engagement training of staff and patients to ensure smooth facilitation of the experience.
Investment of time and funding to ensure proper patient engagement will help drive success – this will be an investment in Health care and a very important one for our future.
This is such an exciting time for health care but one thing we must ensure is that we NEVER get rid of Telehealth Medicare Item numbers that allow a broad range of health professionals to participate in these technologies with appropriate controls on over servicing which so often happens in the health system.
Peter Brooks MD FRACP FAFPHM. is Honorary Professor at the Melbourne School of Population and Global Health and Research Lead at Northern Health.
Brian Oldenburg MPsychol PhD is Professor of Non Communicable Disease Control in the Melbourne School of Population and Global Health andDirector of the NHMRC Centre for Research Excellence in Interactive Digital Technology to transform Australia’s Chronic Disease Outcomes




